EXECUTIVE SUMMARY
- Direct Primary Care (DPC), a subscription-based health care payment model for primary care services, is expanding in the U.S. with many favorable outcomes for both patients and providers.
- While the DPC model may improve quality, accessibility, and affordability of primary care, some detractors note its limitations in health care coverage and argue that the model may prove difficult to scale.
- Further analysis on the DPC model’s advantages over traditional insurance and its tangible impact on the U.S. health care system may be necessary before its wide-spread adoption is encouraged for both patients and providers.
INTRODUCTION
Access to primary care is a key component of achieving the best possible health outcomes for both individuals and communities. Primary care providers (PCPs) foster steady relationships with their patients and serve as a consistent source of care, which is essential for prevention, early detection, and management of diseases and chronic conditions. Regular visits with PCPs are associated with fewer trips to emergency medicine departments, lower rates of preventable hospitalizations, reduced mortality, and improvements in quality of life – which thereby lowers overall health care expenditures.
One major challenge in the primary care landscape, however, is the involvement of third-party billing entities – such as private insurers, government programs, and benefit managers – which may complicate the timely and effective delivery of care. These entities almost always require that PCPs submit detailed documentation and coding of their beneficiaries’ care before reimbursement can be issued. This administrative burden ultimately detracts from the time and quality of care PCPs can afford for each patient – among other adverse effects.
Direct primary care (DPC), is a membership-based health care model that offers a promising solution to many of the problems in primary care. The DPC model reduces the involvement of third-party billing entities, as patients cover the vast majority of their primary care needs via direct contracts with their PCPs. Typically, DPC practices charge flat monthly fees ranging from $50 to $150, in exchange for near comprehensive and unlimited access to primary care services. DPC contracts commonly include routine physical checkups, lifestyle medicine, and chronic disease management; with most DPC practices also offering various lab tests, immunizations, and even prescription medicines at an additional low out-of-pocket cost.
The direct primary care model offers several competitive advantages over traditional health insurance – which makes it a compelling choice for some patients and providers. This insight provides a brief overview of the benefits and shortcomings of the DPC model as lawmakers and stakeholders continue to assess its viability.
TRENDS IN DIRECT PRIMARY CARE
Direct primary care practices are seldom evaluated by academics and lawmakers which makes their adoption and progress difficult to track. Using DPC Frontiers mapper, however, there is evidence to suggest that an increasing number of primary care practices are offering DPC contracts for patients. The number of direct primary care practices has grown exponentially in recent years, from around 100 practices in 2009 to over 2,500 in Q1 2025. These DPC practices operate in 48 states and U.S. territories, serving over a quarter-million people.
While the total number of patients under DPC contracts remains comparatively miniscule to traditional insurance-based models, a 2023 survey of family medicine physicians suggests that direct primary care practices are becoming more popular among PCPs. Eleven percent of physicians surveyed had already been operating a DPC practice or were in the process of transitioning to DPC – which was a significant increase from just 2 percent in 2022.
Congressman Chip Roy, an outspoken advocate for the continued adoption of the DPC model, included in a report some factors that may be driving DPC growth in the country. He cites the Medical Economics 89th Annual Physician Report, which found that 70 percent of physicians surveyed noted that “third-party inference as the biggest challenge” in primary care. With DPC promising to help mitigate this burden on PCPs, the business model could present an intriguing opportunity for providers around the country.
Expansion of direct primary care, however, requires more consideration from lawmakers and health care stakeholders. An exploration of DPCs strengths and weaknesses will help guide discussions on the model’s continued adoption in the health care sector.
BENEFITS OF DIRECT PRIMARY CARE
Access to Timely & Quality Care
Perhaps the most noteworthy benefit of the DPC model is improved access to timely and quality primary care for patients compared to traditional providers. Physicians and other providers at DPC practices tend to have much smaller panel sizes (the number of patients a provider manages) – usually closing after reaching around 800 patients – which means they can allocate more time and attention to each individual patient. Conversely, traditional primary care practices often demand that each provider manage roughly 2,500 patients, which forces PCPs to drastically cut down the time they can spend building a relationship and delivering care for patients. On average, patients receiving care from traditional primary care sources spend around 13 – 16 minutes face to face with their provider, whereas DPC patients typically spend around 40 minutes with their provider each visit. This additional time can lead to more accurate diagnoses, better treatment plans, and improved health care outcomes.
In February, legislation was re-introduced in Congress that promised to provide more leeway in how patients can access direct primary care practices by allowing use health savings accounts (HSAs) to pay directly to DPC memberships. This change would not only allow more people to have access to DPC providers but may also contribute to a reduction in U.S. health care spending. Congressman, Lloyd Smucker, notes that “Allowing individuals with HSAs to pay for DPC services before they enroll in Medicare can reduce the incidence of unmanaged chronic conditions, decreasing federal spending on one of the largest drivers of our national debt.”
Affordability & Cost Savings
1.) Patients
Another strength of the direct primary care model is its affordability for the extent of coverage provided in the contract. For comparison, the average monthly subscription fee for DPC patients ranges between $50 and $150 – far less than traditional health insurance premiums or average out-of-pocket cost for one primary care visit (excluding additional services). To cover for gaps in coverage with traditional insurance – notably certain lab tests, immunizations, and drug prescriptions – most DPC practices provide significant out-of-pocket discounts for patients.
2.) Providers
For providers, direct primary care presents the potential for sizable cost savings by reducing overhead expenses necessary for third-party billing. A primer from 2018 found that DPC practices saved an average of 40 percent on their overhead costs. Another study from 2021 suggests that DPC practices experience more financial stability than traditional providers. This study also cited research that found traditional providers observing a 12.4 percent decrease in revenue in the same period that a sample of DPC providers observed growth of around 13 percent.
3.) Employers
Some direct primary care practices offer contracts for patients directly through their employers, which has demonstrated significant savings when combined with traditional insurance. A case study of a firm that introduced a DPC option for their employee’s health benefit plans, found that there was a significant reduction in total health care claim costs for the firm (see chart below). The savings were in large part due to their employees with DPC memberships having lower emergency and inpatient care utilization. Importantly, the study noted that the introduction of a DPC option increased non-administrative plan cost, however, this was likely the result of other plan changes.
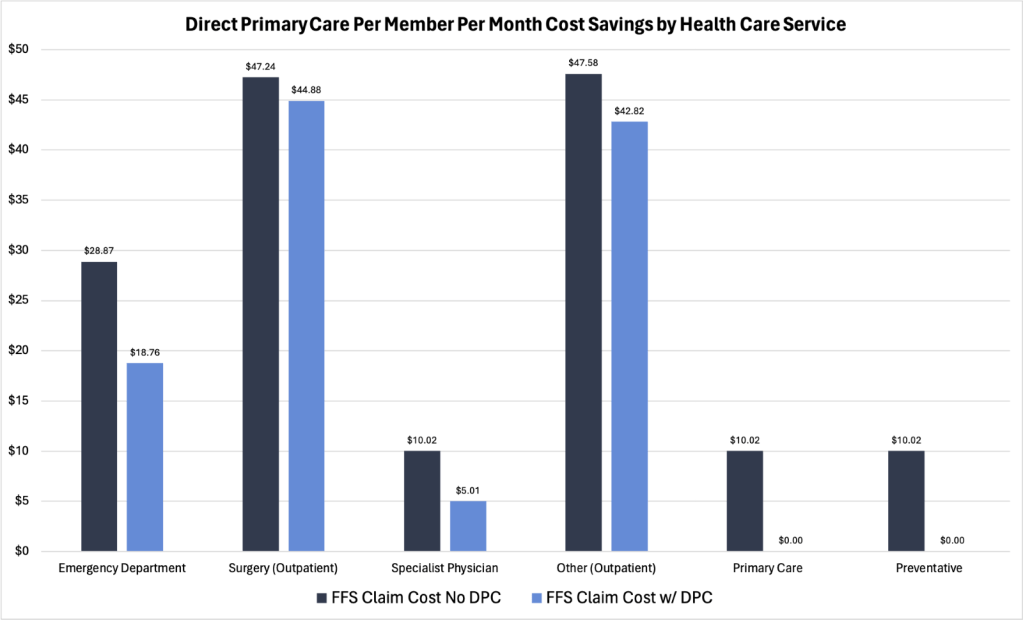
Source: Society of Actuararies (Case Study of Union County)
A study published in the American Journal of Lifestyle Medicine in 2021 found similar findings on employer cost savings when employee health care plans introduced a direct primary care option. The study demonstrated a 54 percent reduction in emergency room claims, and a 13 percent decrease in total medical claim costs. Looking at another case study, it was determined that in the first year of the DPC contract, a county government saved $1.2 million in medical and prescription drug claims – which translated to a $313 per member per month reduction in health care costs for employees participating in the DPC contract.
4.) Government
According to a bipartisan group of Representatives in U.S. Congress, direct primary care may present reduced spending in government health programs – notably Medicare. The premise holds that beneficiaries who utilized DPC practices prior to enrollment will be less likely to need expensive tertiary care, as DPC providers are believed to outperform traditional providers in preventative care and health management.
SHORTCOMINGS OF DIRECT PRIMARY CARE
Scalability
While direct primary care may offer many benefits, some stakeholders have expressed concerns with the direct primary care model’s ability to scale, as well as its effect on workforce shortages. By design, DPC practices operate with far smaller panel sizes than traditional providers, which means DPC providers are limited in the number of patients they can accept. An attempt to increase DPC panel sizes would alter the business model and harm its underlying appeal for most patients. Therefore, the DPC model’s ability to scale is ultimately tied to the number of PCPs, their willingness to operate DPC practices, and their ability to recruit new patients.
Having the requisite number of providers to expand DPC practices is a point of contention in the DPC debate. Critics of the direct primary care model note that given the ongoing physician and health care workforce shortages, and small panel sizes of DPC practices, expanding the model is simply not feasible without enormous loss of coverage. If DPC were to replace traditional insurance, the U.S. would need to triple its workforce in primary care just to break even, according to one estimate. Proponents of the DPC model suggest that the workforce shortage concerns are overstated, as case studies have shown DPC practices decrease health care utilization across many areas of the health care industry. There is also sentiment that the DPC model may improve health care workforce recruitment, as DPC practices are more manageable and less burdensome for providers than traditional primary care.
Coverage Limitations
Although direct primary care covers most needs (about 85 percent) for the typical patient, patients may require supplemental coverage for more serious services – which can result in an increase in the cost of health care. For patients that need more services – such as cancer screenings, surgeries, imaging, and specialty medicines – DPC contracts may not be the most suitable option, even with out-of-pocket discounts. For this reason, relying solely on DPC for health care coverage is not recommended. DPC members commonly combine their subscriptions with high-deductible health plans (HDHP) to cover unexpected and expensive medical bills. Under current law, DPC practices cannot accept subscription payments from health savings accounts, so patients would have to pay for both DPC and HDHP plans.
CONCLUSION
The direct primary care model has, so far, been minimally researched and discussed by health care policy stakeholders. Some experts note many advantages over traditional insurance, including the potential for higher quality of primary care delivery, improved access to primary care services, and significant cost savings for patients and providers compared to traditional insurance. While these benefits support the model’s viability at its current scale, some detractors argue that an expansion of DPC practices is neither practical nor feasible. Further analysis on the DPC model’s advantages over traditional insurance and its tangible impact on the U.S. health care system may be necessary before its wide-spread adoption is encouraged for both patients and providers.
You must be logged in to post a comment.